Med Tech Talks
Equalising access to antenatal healthcare through med techical technology with A/Prof Fiona Brownfoot

Associate Professor Fiona Brownfoot, specialist obstetrician at the Mercy Hospital for Women, clinician scientist at the University of Melbourne and Co-Founder of Kali Healthcare.
Kali Healthcare is undergoing an exciting commericalisation journey and aims to transform pregnancy monitoring through the development of a wearable device that will allow expecting mothers to monitor foetal heartbeats at home.
In her role as Associate Professor of Obstetrics at the University of Melbourne, she heads the Obstetric Diagnostics and Therapeutics Group – a multidisciplinary team of scientists and engineers focused on developing new treatments for obstetric conditions – whilst mentoring PhD students to become the next generation of clinician scientists.
In this episode you will hear about:
More information:
Learn more about Associate Professor Fiona Brownfoot.
Associate Professor Fiona Brownfoot [00:01:14] Thanks so much for all of it and thanks, Sam, for having me today. It’s a real pleasure to be here.
Robert Klupacs [00:01:18] It’s but we’ve been trying to get you on for a while, Fiona. But you’re a busy lady.
Associate Professor Fiona Brownfoot [00:01:21] Oh, not at all. I’m just really grateful and excited about today.
Robert Klupacs [00:01:25] All right, Fiona, let’s. Let’s start at the very beginning of career. As I mentioned, you have a Bachelor of Medicine and Bachelor of Surgery from Adelaide and a Ph.D. from Melbourne. What got you interested in obstetrics? And why did you choose to specialise in this particular field?
Associate Professor Fiona Brownfoot [00:01:41] Yeah, sure. So, it was really during my medical school days where I became interested in obstetrics, and it was really my mentors, Professor Dustin Baker and Professor Caroline Crowther, who were both heavyweights in in research in obstetrics. They got me interested. I actually wrote a Cochrane Review with Professor Caroline Crowther, and it was really that that stemmed my interest in obstetrics and made me realise just the deficiencies of treatments and diagnostics within obstetrics. And this is an area whereby we could really improve the care through research. So, it’s both a combination of having an interest in obstetrics, but also knowing there were these deficiencies in the field. And I had had quite an interest in research that really drove me down that pathway.
Robert Klupacs [00:02:27] The other thing is in recent times, Kali Health Care, it’s been making some very big waves in the medical industry here in Melbourne. You’re a co-founder. Can you explain to our listeners how Kali came about and what the unmet clinical need you seek to address is?
Associate Professor Fiona Brownfoot [00:02:42] Yeah, absolutely. So, the idea behind Kali Healthcare really came from the clinic. So, recognising that there was deficiencies in the way that we’re monitoring babies and this really came about as the moment we use ultrasound machine Doppler machines in order to pick up that baby’s heart rate in women at high risk of stillbirth and there was just problems with the current technology. The Doppler has to be placed directly over the baby’s heartbeat in order to pick up a fatal heart. So, the mother must be lying down. It must be placed by a clinician, a midwife or obstetrician. So, it’s placed directly over that heartbeat. And then the woman can’t really move around because if the woman moves or the baby moves, then it can lose that position and move away from that foetal heart and then we get signal loss whereby we don’t know exactly how that baby’s coping. Equally, it can move onto one of the maternal blood vessels and stop picking up the mum and in fact, a number of stillbirths, 40% of stillbirths, which she referred to, the FDA sort states that that confusion between foetus and mothers as one of the driving factors behind stillbirth in those cases. So it was both that technology and wanting to improve that technology to make mums more mobile so that the signal wouldn’t drop out and say there was no maternal foetal confusion. But it was also the prospect of having a technology which might be able to be moved into the home and really equalising care for women that aren’t at centres such as tertiary sites where there’s a lot of clinicians. So it was really those aspects of frustration with the current system that really drove us towards how could we better monitor our mums and give our mums a better experience and also equalise health care? And it was in partnership with the electrical Engineering department at University of Melbourne and Professor Palaniswami, and we brought on a joint PhD student who’s an electrical engineer, Dr. Emerson Keenan, whereby this project really came to light and it was really driven by Emerson and his Ph.D. and it was absolutely a combination of the medicine and the engineering together that we really needed to go together on this project in order to be able to develop this new technology and this new device in order to have a device that’s portable, wearable and could potentially be used at home.
Robert Klupacs [00:05:07] So how does it actually work?
Associate Professor Fiona Brownfoot [00:05:08] The device so the device picks up the electrical activity of the baby’s heart. And look, it was a really complex problem because the electrical activity of the baby’s heart is very low amplitude. And there’s a lot of electrical noise coming from the maternal heartbeat. The got mobile phones, you know, external electrical activity. So initially we had to find where is going to be the best position to put the electrodes in order to best pick up that fatal heart. And this really came down to a large clinical trial where we recruited 100 women and we determined where abouts the baby’s heart was in relation to other maternal factors. And surprisingly, we found it was just about always around the umbilicus or within a couple of centimetres of it, regardless of if the baby was breech or head down cephalic and I think that’s because babies have a huge head compared to their body, which is quite different from us adults. But it meant that that heartbeat was always around the umbilicus, which is good in many ways, as it means that those senses needed to be positioned on the side of that umbilicus. So then the next step was placing a huge amount of sensors, so 24 sensors over the maternal abdomen of 50 women in order to see exactly the number of senses that could pick up that heartbeat really accurately. And also, the location of those sensors, which really helped guide device design and in the sense of patch. And then it was working with engineers at Neo-Bionica that helped us design the hardware. And the hardware is smaller and lighter than an iPhone that sits on the maternal abdomen, making this device completely wearable and portable, which means that we no longer need that huge infrastructure of these foetal monitoring units that hospitals currently have and means that then we can decentralise care and allow these women to have monitoring at high cost. In many ways, COVID has been, I mean, a real challenge first, because you couldn’t recruit patients, but it has opened up those pathways to at home care in ways that I never could have anticipated and perhaps might never have been possible without a pandemic that really demanded at home decentralised care. So now MDS codes available fit for telehealth. And there’s now a number of countries which have moved towards this hybrid model of half care in hospitals and half care at home or indeed hospital in the home set up. Robert Klupacs [00:07:35] Wow. That’s amazing. Absolutely amazing. So how confident are you that your system can discriminate the foetal from maternal heartbeat regularly, consistently with enough clarity so it’s going to be effective for the mother?
Associate Professor Fiona Brownfoot [00:07:48] Yeah, that’s a great question. So, the maternal heartbeat has a much higher amplitude than the foetal. So, in fact, that doesn’t seem to be a problem with the electrical device that we have. But perhaps it’s more the accuracy of the fatal heart rate that we needed to optimise. And we did that by recruiting those women to develop the device in the certain layout and, and design that we have. And then we needed to recruit women to the clinical trial to see whether or not we could develop algorithms that helped us extract that foetal heart. And we used traditional algorithms which unfortunately fell short. And it wasn’t until we used artificial intelligence, we showed we put the traditional ultrasound based monitor on these women and in the electrical device on these women, and we showed the computer the seat readout, and then it learnt from the electrical activity how to develop a trice similar to the current traditional technology listeners.
Robert Klupacs [00:08:47] Because Fiona is making this sounds so easy. I know it wasn’t.
Associate Professor Fiona Brownfoot [00:08:51] Can I tell you; it was so incredibly difficult. And in fact, the engineers, Emerson really was behind developing these really novel algorithms. He said to me, Fi, it’s a bit like the Olympics of engineering. I feel like this is not basic coding, like this is really quite complex and we didn’t even know if it would be possible. And in fact, we thought it would just be a research paper. If we can’t better those traditional algorithms is the FDA requires more than 80% accuracy within 10% of the site of the foetal heart rate detected on the CTG. But in fact, with the novel device design and the algorithms in our validation cohort, we were able to get 90% agreement, which is well above that 80% FDI standard.
Robert Klupacs [00:09:36] So listening to you, it sounds like it’s done or.
Associate Professor Fiona Brownfoot [00:09:39] There’s a long way to go.
Robert Klupacs [00:09:40] Yeah, I know. I was teasing you, so maybe you could tell us what the next steps exactly.
Associate Professor Fiona Brownfoot [00:09:43] And this is so a little tame once we got these results that in fact it was 90% accurate and indeed it exceeded the expectations of the regulatory bodies, then we knew we had something, and it was something really exciting that then could be taken to the clinic. And we celebrated for 24 hours and then the commercialisation mountain appeared in front of us and we thought, right, we’ve got to get this technology to the patients. It’s the whole reason and we’re doing this, and we want a better outcomes. We want women to have a better experience. There are women at high risk of stillbirth. And so, it was at 24 hours we celebrated. Then that mountain arose in front of us. Now the outcomes are actually commercial outcomes. We need a startup. We need commercial based funding.
Robert Klupacs [00:10:31] Yeah. So, you’ve raised $1,000,000, which, Congratulations.
Associate Professor Fiona Brownfoot [00:10:34] Yeah. Thanks so much.
Robert Klupacs [00:10:35] How hard how hard was that?
Associate Professor Fiona Brownfoot [00:10:37] Huge relief. Oh, look, it’s tricky, and but I’ve got to say it, I feel that the commercialisation landscape in Victoria has changed substantially since we started this project. So, this was really a research project that started five years ago, and in that time I’ve really seen a shift in the Victorian Start-Up ecosystem whereby it seems that there is a lot more funding, especially in these Pre-seed stage. It seemed that before you could get research funds and you could get funds for develop technologies for clinical trials, but there’s this huge valley of death in between in that TRL stage prior to the clinical trials, like after the research, but prior to those big clinical trials.
Robert Klupacs [00:11:18] So what was it enabled you to close the first 1 million? Was there some particular data point that the investors needed to see or.
Associate Professor Fiona Brownfoot [00:11:24] You know what, it was a range of things that we needed to achieve. So absolutely, we had to show that we had evidence that indeed we had a technology that was accurate, and we had to show them the vision of the technology that we would then commercialise. And we were very fortunate to get a Neo-Bionica proof of concept voucher which allowed us to develop the hardware in a design that we would then look to develop the commercial grade product in. And it was also with the medical device partnering program and the team in Adelaide, which helped us design the board to fit that enclosure. So, it was both having that strong research evidence as well as a prototype to show investors that allows us to then seek that pre-seed funding. And it was also more than that. It was having a business case and also having a business case as well as speaking to consumers and stakeholders. Yeah, so it was only once we had done that further investigation whereby we interviewed 70 women who were at high risk of stillbirth, who were having traditional monitoring to get their opinions on a portable wearable device, as well as their opinions on at home monitoring, coupled with 50 clinicians, both midwives and obstetricians, and getting their opinions on both the wearable technology and their feelings of an at home monitoring device that were able to put together a robust business model and plan that we could then go to investors with.
Robert Klupacs [00:13:05] So just out of interest. So is the stage to get the product approved and come back to that.
Associate Professor Fiona Brownfoot [00:13:09] Yes.
Robert Klupacs [00:13:10] But right now, if you get the product approved, so women at the target market is women at risk of stillbirth. And I’m assuming you as an obstetrician can identify them fairly early, is that right?
Associate Professor Fiona Brownfoot [00:13:19] Yeah, that’s exactly right, Robert. Yes. So, look, around 50% of our women will have a CTG that’s a heartbeat monitor during their pregnancy and the main reasons is reduced foetal movement. So, the mum comes in to hospitals, says “My baby’s just not moving”, and then you put that heartbeat monitor on to pick up that fatal heart to see whether indeed the baby’s in distress and needs urgent delivery or in fact, the majority of the time babies are actually doing well and it’s just change positions and the woman can continue the pregnancy safely. But we don’t know that until we’ve got that foetal heart rate monitor. Women with diabetes, women with high blood pressure are all at risk, requiring foetal monitoring. And then indeed, 80% of our women will have foetal monitoring in labour. So that’s the vast majority of our pregnant population. Vast majority of our population is needing monitoring at some stage in their pregnancy.
Robert Klupacs [00:14:09] Imagine your investors would have asked you this, but so who’s going to win the products approved? Yes, and it’s available by manufacturers. Who’s the buyer? Is it the mother or is it the hospital? Who’s going to be the payer for this?
Associate Professor Fiona Brownfoot [00:14:21] So at the moment where it’s a clinician-based model because we don’t want it to be used incorrectly, the woman putting it on at home, activating it herself, not knowing if it’s a reassuring price or not, because there’s a lot of intricacies that go into creating that heartbeat monitor. So, at the moment it will need to be clinician approved and it will be the clinician that either purchases device or indeed the hospitals that purchased the device. There is this green field market, there’s currently not a device that can be used for at home monitoring that’s activated by the clinician. So, there’s plenty of doctors out there, those ultrasound based ones. But quite often those women are getting confused that the hearing their own heartbeat reassuringly and not hearing the foetus. And indeed, by just putting that Doppler on, you’re not getting that readout of the fatal heart to know if that pattern is indeed reassuring or not.
Robert Klupacs [00:15:13] When the woman comes in the you would sell them, or would you have bought that and then handed it to them? Is that how it works? So, you there’ll be a manufacturer of these devices? Made available to clinicians?
Associate Professor Fiona Brownfoot [00:15:25] Yes.
Robert Klupacs [00:15:26] And the clinicians then sell that to the mother.
Associate Professor Fiona Brownfoot [00:15:29] Yeah, exactly right. So, at the moment we’re thinking that it would be the clinician owned, so it would likely be bought by hospitals. Okay. Or private clinicians. And then those hospitals would then have a set up whereby that put it on the women while they’re waiting for the antenatal appointment. So, you wouldn’t need the big foetal monitoring units with all the beds in the cubicles anymore. They could just in fact wear it while they’re waiting. The women can put it on themselves and wear it while they’re waiting, or indeed it could be something that’s loaned to the woman during their pregnancy that same returned. I think that seems the way things are moving. I think in the future perhaps it will be patient led, given that’s the way our watches monitor, our heartbeat. Google has all the information about our heart rates and things, but at the minute we’re really focused in on a clinician based system that’s operated by them. Its junction with the woman.
Robert Klupacs [00:16:23] It’s fascinating, I remember there was a study about how many births there were in Australia the last few years. I think yes, on average is about 300 to 350000 births a year.
Associate Professor Fiona Brownfoot [00:16:31] Yeah, correct. Yes, about three. 300,000.
Robert Klupacs [00:16:33] So how many of those women do you think are likely to need your particular device.
Associate Professor Fiona Brownfoot [00:16:38] To monitor the vast majority? Yeah. So it’s 50% of those women will need monitoring during their pregnancy at some point in their pregnancy. The letter present with reduced movements, high blood pressure, diabetes, obesity, they’re all risk factors for which those women might need to be monitored. And then indeed in labour, by far the majority of women and now having continuous foetal monitoring in labour and the current system is quite suboptimal, we’ve got to continue to reposition it, the midwife troubleshooting the technology rather than being with the woman in labour. Yeah, but pinning the woman to the bed when in fact the woman quite often wants to be active in labour. So a device which is wearable and portable where the midwife isn’t troubleshooting, are we picking up the mum or the baby that’s accurately picking up that fatal heart rate I think would be really beneficial.
Robert Klupacs [00:17:26] Sounds like a fantastic product question. And I’m just as I’m listening to you, so what’s the next step? How do you go from where you are at the moment? To get it to FDA approved stage?
Associate Professor Fiona Brownfoot [00:17:36] Yeah, absolutely. So at the minute that 1 million in funding. So we obtain that from the Genesis Fund, which is through the University of Melbourne. It’s a Pre-seed fund and Alice Anderson is a fund that is really directed for Start-ups with women founders as well as some private investment so able to close that million dollar round. What that allowed us to achieve is development of the commercial grade device, along with the regulatory paperwork for the hardware and software of that device. And Neo-Bonica assisted us with developing that hardware and Two Bulls, which has now changed its name to Dept, has helped us produce the software. And so now we’ve got a commercial grade device which is being put together as we speak. And on the 1st of November we’ll have the first commercial grade device. That device will be available to sell to researchers who are researching in stillbirth, which it will just be fabulous. I think the impact this could have is far greater than the clinical trials I’ll run. You know, he’s hoping it go. You know, it’s available to still best researchers worldwide to help us better understand stillbirth and fatal monitoring. But so we’ll have that commercial grade device it in the next step is to clinical trial in order to get regulatory approval through the FDA and TGA. And we’re currently in consultation now where we’ll have a pre submission to the FDA to sit down and talk to them about how we plan our clinical trial to look and whether or not they would have any recommendations for us before we embark.
Robert Klupacs [00:19:04] And presumably go to make it large enough so you can get some health economic outcomes compared to some historical controls. I suppose.
Associate Professor Fiona Brownfoot [00:19:11] You’re correct. So it will really be around the accuracy of the device, these trials whereby we need to prove to the FDA that indeed it has an accuracy greater than 80% of the time being within 10% of that CTG monitor in order for to get a 510 K approval through the FDA.
Robert Klupacs [00:19:31] Wow. How long do you think that’s going to take?
Associate Professor Fiona Brownfoot [00:19:33] It’s a very easy study to enroll patients in. So already patients are quite willing to be enrolled, both pregnant patients as well as labouring women. I think they understand the troubles and difficulties with current technology. So we’ve enrolled 200 patients over two years and I think that in fact it will be perhaps less time to recruit women to an FDA study with a commercial grade device.
Robert Klupacs [00:20:00] I hope we’ll listen to start invest. It sounds like a fantastic opportunity.
Associate Professor Fiona Brownfoot [00:20:03] Oh, thanks, Robert.
Robert Klupacs [00:20:04] Yeah, it’s a little change, a little tack, a little bit more about you now, Fiona, We’ve had many clinicians turn entrepreneurs on this podcast. I think about ten now, I think, and I’m really keen to hear why you chose that particular path, because it’s not for the faint hearted. Was there a defining moment that you might that made you say to yourself, This is something I need to do?
Associate Professor Fiona Brownfoot [00:20:24] Yeah, it’s, you know, it really was. And it was really in the clinic that drove me back into the laboratory to undergo research studies. So it was it was a patient who had pre-term pre-eclampsia. And five years earlier, she had preterm pre-eclampsia. She needed delivery of that baby. And that baby ended up with all of the complications of prematurity, including severe cerebral palsy. And really, sadly, this time around, she developed pre-term pre-eclampsia and unfortunately, she suffered a stillbirth with this baby. So it was really that she asked us, surely something has changed in the last five years. Surely something can be done to help me so that I don’t have to have this baby preterm and run all of those risks. And it was really her, along with a number of other women, training women that are at high risk of stillbirth and being in the clinic and seeing the deficiencies in current technology. So for instance, CTG machine was made in the 1970s and eighties and it really hasn’t changed much. So seeing those deficiencies then is a real driver towards we’ve got to make a better, safer environment for our next generation, for our mothers and our babies.
Robert Klupacs [00:21:41] So then how did you find Emerson and the guys in electrical engineering?
Associate Professor Fiona Brownfoot [00:21:44] Yeah, it is quite a cool story. So it was one of my colleagues. He’s was friends with one of Palaniswami’s friends and he knew that I was interested in foetal monitoring. Palaniswami was also interested in foetal monitoring and had been working on foetal monitoring for a number of years and he traduced us. And it is honestly the synergy in skills which has allowed us to develop this device that we are now looking at translating through to the clinic. I think it’s been absolutely essential to have people with a shared interest. I think if I just approached any engineer and I hadn’t had an interest in fate, you know, it’s a hard thing to kind of get into this exciting, remarkable pregnancy complications, you know? Yes, he’d already had that interest, which I think was a huge driver.
Robert Klupacs [00:22:32] As you say. We’ve had a few questions on this, but. And we know quite a few of them and they talk that, oh, there’s all these problems, but you’re a bit different. You made the jump to be entrepreneurial, to do something about it. And I know there’s a lot of them frustrated. Would like to do what you’ve done. What advice would you give to your clinician colleagues because they still want to earn money? Yes, they’ve been trained heavily. I see a problem when they’re passionate about helping their patients, but they don’t quite know how to go about it. So you seem to have been able to do that.
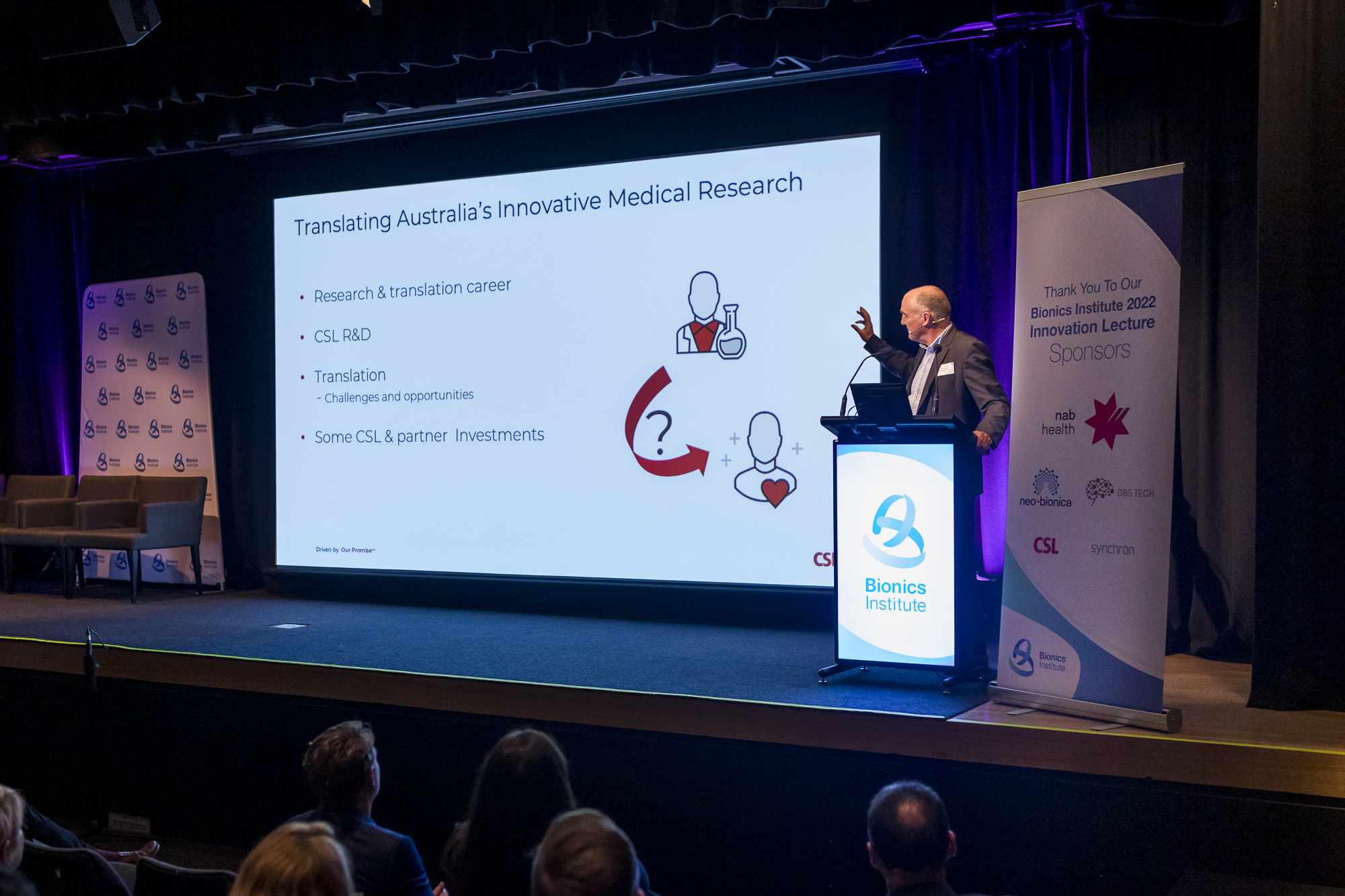
Associate Professor Fiona Brownfoot [00:22:58] Oh, what their Robert has been navigating these 4 to 6 years, like since I finished my Ph.D., I wanted to look at novel device development and it’s in finding the right mentors, I think is the best advice. So I had a mentor. I still have a mentor, Professor Greg O’Grady, and he’s in New Zealand and he developed a monitoring device very similar to what we’re doing, just monitoring the gut rather than the foetus. And then it was also in Mark Cook. So I was introduced to Mark Cook, who is developing epilepsy monitoring devices, and again that is really similar in actual fact, and that’s how I got onto our friends at Bionics and Neo-Bonica, and it was in connecting with those people that gave me the know how in order to progress this, as well as having engineers that are absolutely invested and interested in the subject matter and really kind of hoping to inspire them to keep them along that same trajectory to develop a device that could assist us in the clinic. So I think mentors absolutely key made as many people as you can and then work out who has the know how in order to help progress things. generally, they are so happy to chat and so happy to help in any way they can.
Robert Klupacs [00:24:20] Yeah, I think it’s because everyone likes you.
Associate Professor Fiona Brownfoot [00:24:21] Are you so nice Robert!.
Robert Klupacs [00:24:23] That they don’t help everyone.
Associate Professor Fiona Brownfoot [00:24:25] Oh, that’s it. Well I am. Yeah. I think that’s the other thing you know, you’ve got to think about it is working with people you enjoy working with. I think otherwise collaborations just fall apart. If you can’t kind of have a laugh together because it’s a hard road with many roadblocks.
Robert Klupacs [00:24:42] So you actually pick up mentoring. So I know that, yes, I can imagine Now people are coming to you as part of this mentors. What do you think makes a good mentor? Because this is something we’re really trying to pick up on this podcast.
Associate Professor Fiona Brownfoot [00:24:52] Yeah, absolutely. So I think for me, I think a good mentor is somebody that’s got a shared interest and it might not be in the same field. So but at least a shared interest in a technology or a research area that you’re also interested in. I think that someone who’s a connector is also really important. So a mentor who can say, “Have you seen this grant? This is how we went about it. How about you talk to this, this group of people”, They might have the skill set that will help kind of push this project forward.
Robert Klupacs [00:25:26] The other question I’m.
Associate Professor Fiona Brownfoot [00:25:27] Trying to think of all the things that.
Robert Klupacs [00:25:29] I will come to you later on. It’s okay.
Associate Professor Fiona Brownfoot [00:25:30] I know this is the problem.
Robert Klupacs [00:25:31] I don’t want to lie. I think I think I think you ask that really great.
Associate Professor Fiona Brownfoot [00:25:34] Short like he’s been so and Mark Short.
Robert Klupacs [00:25:37] And Greg and.
Associate Professor Fiona Brownfoot [00:25:38] And Greg exactly like I yeah I think they have been absolutely instrumental in connecting me with that MedTech environment and I think it has a lot to do as well with the infrastructure and the environment that you’re in. I think in Victoria we are so lucky now to have that the Bionics Institute, Neo-Bionica with that people with that ISO 13, 1345, we’ll see manufacturing capabilities and things in order to drive it.
Robert Klupacs [00:26:07] Question A few people asked when you were coming on today, you’re an entrepreneur, you’re a car carrying OBGYN. Yeah, you seem pretty healthy, but we know there’s only 24 hours in the day. How do you juggle at all?
Associate Professor Fiona Brownfoot [00:26:21] You know, all of it. It’s a team. It takes a huge team and there’s ten in my team. So I have the Obstetric Diagnostics and Therapeutics group at University of Melbourne and I’ve got two postdocs, a science and engineering post-doc like Emerson’s now the CEO of Kali Healthcare, so now my boss, it’s crazy how you got to train your students. Well, because one day I might be your boss as well as research assistants, midwives, and I’ve got four PhD students as well. And it’s really teaching that next generation of scientists, clinicians, engineers, the intricacies of obstetrics to drive the research forward and drive these ideas from just a research project or paper, but actually drive them to the clinic. And the only way you can do that in med tech is through is really through commercialisation, and it’s the patients that are the huge driver source up plus not for delivery of patient and it’s getting better outcomes for our mums and babies.
Robert Klupacs [00:27:23] Fantastic. So you know, I’m listening to you your whole career trajectory, I can’t believe it. But did you start out, you know, as a young girl at high school thinking this is where I’m going to finish up. If you could go back in, if you could go back and talk to that young girl. What would you say to her?
Associate Professor Fiona Brownfoot [00:27:38] Yeah, sure. I never could have envisaged that this is where I’d be. And I think go with your passion and what inspires you. And it’s really that that doesn’t matter how long you’re working because you love it and you just enjoy it so much and it becomes a part of your fabric, really. So I think, yeah, the best advice I can have would be, you know, make sure that you’re on that path with things that inspire you and things that you really enjoy.
Robert Klupacs [00:28:06] The way in college, successful in whatever it is, one year, two years, three years time, and you’ve got the product on the market. FDA approved. What’s going to be the next challenge for you, do you think?
Associate Professor Fiona Brownfoot [00:28:17] So many challenges and, you know, exciting problems to overcome. So I guess with the Kali Device, we’re looking to see whether or not it might indeed help us detect preterm birth better. So preterm birth occurs in 10% of pregnancies. We’ve got a swab test that lets us know if preterm birth is unlikely, but it’s only accurate 50% of the time to tell us if these women will labour and we anticipate there might be an electrical signature in the uterus that the Kali Device might pick up that will allow us to detect if these women will indeed go on in labour and optimising it for use in twins. So there’s still a huge amount of work from a colleague perspective to then, you know, put in motion. And then of course we would then need to put in further regulatory submissions, but at least knowing how to achieve it. And that pathway I think has been absolutely invaluable as well as looking at computerised analysis, in which case these women might be able to then use this device at home on a plot themselves and then, you know, engage with the midwife if indeed the computer is picking up that it’s abnormal. I think that’s kind of the way things are running. It’s decentralised and less clinician intensive care.
Robert Klupacs [00:29:36] I mean, we all live in this wonderful country, Australia, but I know a little bit about this, but I’m interested in your feedback. So the number of stillbirths in this country, particularly in particularly subpopulations, Yes. How many is there? And, you know, everyone assumes that there’s lots of healthy births and yes, it’s nothing to worry about. But let’s just finish this off. This is put in perspective for what you were trying to achieve, why this is such a problem for so many people.
Associate Professor Fiona Brownfoot [00:30:00] Yeah, of course, the stillbirth rate in Australia is one in 140 pregnancies. That’s a lot. It’s. It is a lot. It’s why higher than our road toll. And yet it’s something which I think is starting to be spoken about that traditionally hasn’t really hit the headlines like the road toll has. So we’re really trying to focus on improving outcomes for these women and making their pregnancies that much easier, having a wearable technology they can use at home, being monitored at home rather than being hospitalised.
Robert Klupacs [00:30:31] Is that the same throughout the world? Because I hear and what I’ve read was in particular in the United States like us, a great country, but in certain populations of the United States, the stillbirth right is much higher than.
Associate Professor Fiona Brownfoot [00:30:41] One or even higher. Yeah, correct. I think we’re very lucky in Australia to have universal health care. And that’s right, places that don’t have universal health care. Unfortunately, those outcomes are worse or indeed it is something that would look at commercialising globally.
Robert Klupacs [00:30:56] Oh, that’s fantastic, Fiona. We could talk all day.
Associate Professor Fiona Brownfoot [00:30:59] We could.
Robert Klupacs [00:31:00] We can’t, but we know you’re a busy lady, so we thank you very much. We’ve reached the end of the podcast. So for a woman that’s finished giving look, giving, doing a delivery fur AM look remarkably healthy.
Associate Professor Fiona Brownfoot [00:31:11] Keeps me going!
Robert Klupacs [00:31:13] And for us was a fascinating discussion. I suspect for our listeners, you’ve given us a lot of stats that a lot of people didn’t know about. The fact that what you’re doing can make such an impact is amazing and the fact that you on the journey and it doesn’t seem that far away from hopefully having a successful product. So thank you for everything you’ve done. Yeah, we wish you all the very best success in what you’re doing. And our listeners, I’m sure if you wanted to invest Fiona or take your phone call.
Associate Professor Fiona Brownfoot [00:31:37] Yeah, absolutely we will. Or if you want to join us along the journey, the commercialisation journey. Very happy day. You never know who’s listening.
Robert Klupacs [00:31:46] So thank you again, Fiona. To our listeners. I hope you enjoy listening and I look forward to introducing you to our guests in future podcasts. There are links to everything we talked about in the show notes and we look forward to welcoming you next time.
Listen to other episodes of Med Tech Talks here