Med Tech Talks
Dr Andreas Fouras, Founding CEO of 4DMedical – Bionics Institute 2023 Innovation Lecture special
Dr Andreas Fouras and his team have developed a unique respiratory imaging system, which aims to change the outcome for patients with lung disease.
In 2012, Andreas founded 4DMedical to commercialise the technology, which is now an ASX listed company.
In his keynote, Andreas illustrates his entrepreneurial journey, speaks about the highly innovative technology at 4DMedical and shares some of his thoughts about innovation in Australia
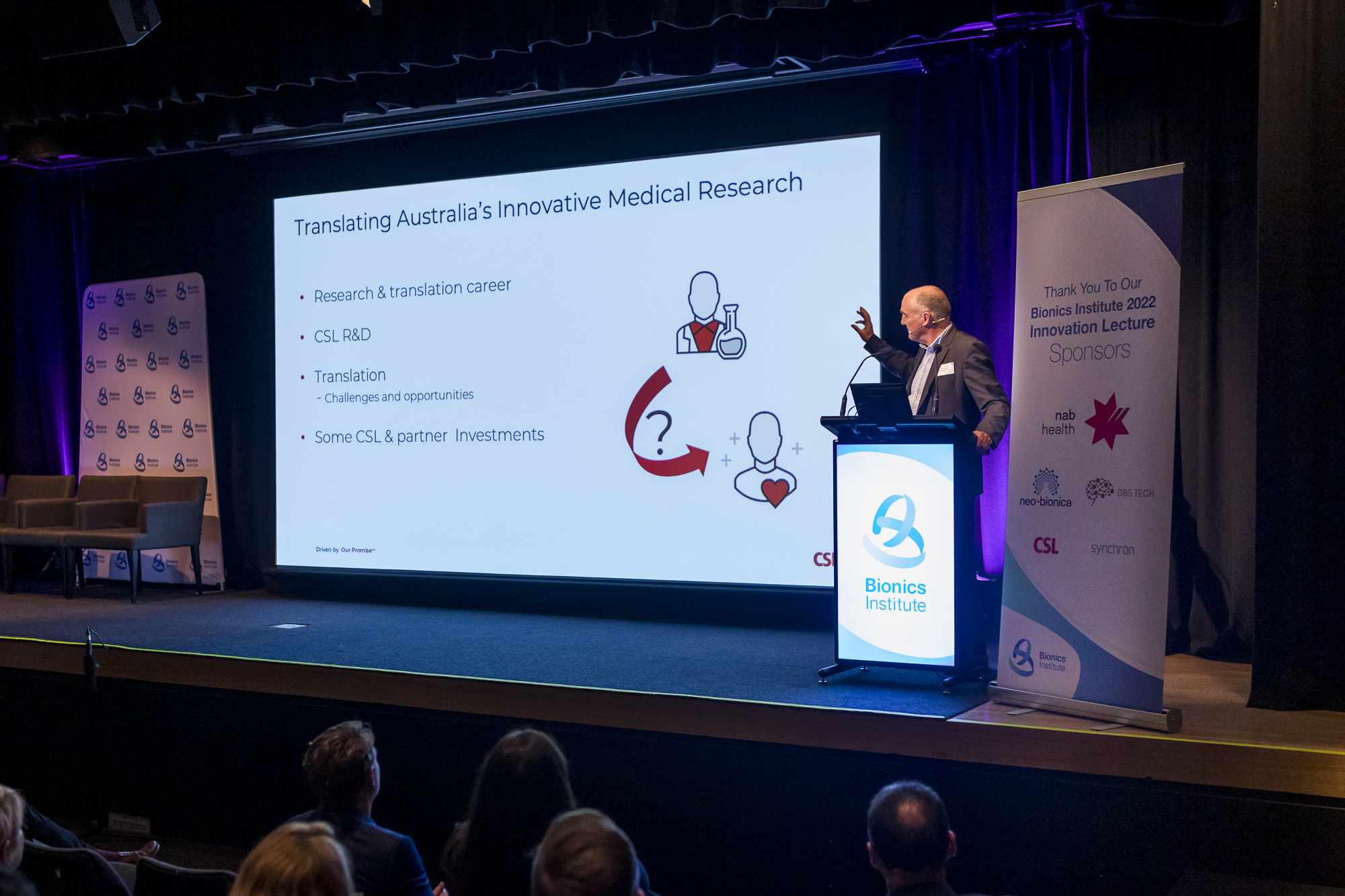
Over 320 guests comprising med tech executives, researchers, clinicians, government staff and investors attended the Bionics Institute 2023 Innovation Lecture to explore how Australia can accurately measure innovation, boost the med tech ecosystem and strengthen connections.
More information:
Watch the Bionics Institute 2023 Innovation Lecture recording
Dr Andreas Fouras [00:00:38] Well, this is an incredible honor. I’m I’m really just super stoked to have the chance to share some of my thoughts on this. And that will somewhat compensate for the significant kind of backward step this is doing to my own imposter syndrome work that I’m doing in the back in the background. I’m. So I just have a few little points while while you’re looking at some of my favorite pictures of lungs breathing in the in the background. I think one of them is we really have to think about innovation and what it means and where it sits. And as someone who’s, you know, an inventor and an engineer, I feel that the current definitions both rule out and also let off the hook. Everybody else who isn’t doesn’t fit into that scientist or engineer category. We can be innovative about the way we fund things. We can be innovative in the way we organize people. We can be innovative the way we create metrics. And all of those forms of innovation can really help us do a better job. Certainly at 40 medical, we say we say all the time that innovation does not end with the product we take. It’s how we take it to market, how we deal with each other. Another quick point is that, you know, I guess I’m incredibly pleased that just recently, you know, 40 Medical has been doing really particularly well. We’re well funded. We’ve we’ve recently raised another $20 million. So I guess I get the opportunity to be able to talk to you today from a position of success. So it doesn’t have to seem like I’m complaining from, you know, one of the one of the beaten down masses. But at the same time, I often I really do sometimes think it’s remarkable that we got here. It’s you know, I’m quite shocked sometimes that we’ve gotten to this point. So I guess I wanted to give you both of those. And then finally, when we’re talking about solutions and and I absolutely loved the previous talk. Thank you so much. And I just want to say, if we’re arguing about whether it’s an increase of 6% on something is enough, and that’s the conversation. It’s like that is the wrong conversation. We are missing zeros from the solution here. The the the where the situation is is costing this economy, this country and the federal budget and the state budgets, if that’s where we have to bring it down to tens and hundreds of billions of dollars and $50 million solutions are not how you solve $100 billion problems, at least not not in my opinion. So sorry about about that initial kind of kick off. Thank you. And so very, very proud about what what we’re doing and how we feel that the technology we’re developing at 4D really can be an Australian led change to lung health. But I also thought I’d change the title to this instead. And I do feel like it’s okay that it’s hard. But honestly, as someone who is who is progressing through it and at the moment at a peak on the roller coaster, I really don’t think it has to be as hard as this. We can do better and we can. We owe it to the people who are behind me in the list, ready to come through to make it easier than this. And if we do that for them, they will reward us ten times over. So. So why why is 40 medical for the Simon Sinek fans amongst us? And quite simply, we are being failed. Existing lung diagnostic technologies are failing us. And that might seem surprising to some of you that that’s that that’s the case. But it’s actually really, really easy to prove I can do it. I think in about 15 seconds, I have met some of the world’s best lung doctors, the best minds in lung health, and on a regular basis, they struggle to see what’s happening inside of their patients lungs, whether it’s to detect the disease in the first place or to track its progression every single day. So let’s give some examples. I think a really easy place to go to is is lung cancer. Let’s look at lung cancer. It’s and, you know, the statistic will vary depending on where you are and what year. But lung cancer is about the fifth most common cancer. Right. But it kills more people than number one, Number two and number three combined. Why is that? It’s because we don’t know what’s happening inside of people’s lungs. It takes us too long to see it. That’s at least a contributing factor. And here is a I’d like to go immediately to it. To a human. Sorry. Sorry. It is when I move around. Is that making me Lateran? Quite okay. So I’d love to share with you Amy story and in a way that if you can see inside someone’s lungs and you can understand what’s happening, how that can, you know, how that can help, you know, the that patient on that day. Amy [00:05:39] In 2021, we realized that our family had come down with COVID and several days in my husband and my daughter were starting to feel better and I was not. I had no energy. It went on for a couple of months. Nobody knew what was wrong with me. Doctor [00:05:58] She came in, she said, Look, I’m not myself. Something really is wrong here. But all the tests came out normal, and she had been to see multiple doctors and she wasn’t getting any better. Amy [00:06:09] And I had so many scans and X-rays, and none of them showed why or how I was sick. Dr. Kashkari called me one morning and he says, Amy, calm down. I want you to do this for a scan. Doctor [00:06:24] I said, There’s a brand new test. It was the 4D medical Zombie Lobos test. And this test is FDA cleared. I’d like you to have it to see what it would show about your lungs. Got the test back, and it was really surprising because it was markedly abnormal. Amy [00:06:41] He called me later that week and said, Amy, you’re very sick. And I said, Oh, finally, someone believes me. Doctor [00:06:49] Normally, patients don’t want to hear their test is abnormal. She was surprisingly happy to hear her test was abnormal because it meant that, okay, there’s somebody found something wrong here. It showed the defect and none of her other tested. Amy [00:07:07] It’s just amazing. It’s like magic. You can see it right there. What is wrong? It felt so good to know that I was not crazy, that there was really something going on that needed to be treated. One day I woke up after the scan and after the proper medications and I thought, I’m back. I had energy. It changed my life. It’s amazing. Dr Andreas Fouras [00:07:43] So I think that obviously if you don’t have the right information, you can’t make the right decisions. And, you know, we need the right decisions to drive the best the best outcomes. But very quickly, talk to you about the framework of what the existing technologies are that are out there right now, that are that are currently that we’re currently using to understand what’s happening inside of folks lungs. And they are, you know, a one dimensional test and a technology that gives that gives us single numbers that describe what’s happening in our lungs invented in the mid 1800s. We have X-ray technology that was that was invented in the late 1800s and then really turned to medical field in the mid in the middle of the 1900s. That gives us a flat, single two dimensional image in black and white of what’s happening in our lungs. The most commonly delivered test is that if you think about what else in your life you would tolerate, that was flat, still black and white and two dimensional. Let let me know if you can if you can think of something and then you have the CT scan, which is the new great new high tech thing in in. Sorry. That is. Anyway, so there’s a little story here. So city was clearly not that seat and it’s not an x ray. So it was invented in the in the 1970s. Right. So also just simply not you know that gives us once again, a still image of how our lungs look, not how they appear. And for me, an analogy of that is if you had a problem with your car and you know, you took your car to a mechanic, the mechanic said, Pop the hood, took a photo of your car engine, send that photo to a friend of his who looks at car photo engine pictures for a living and then said, I don’t know what’s wrong with your car. That’s that’s kind of how it’s working today. 40 Medical provides a moving image of how the air moves within your lungs as you breathe. It shows how your lungs work as they breathe, which is really what the problem is. It’s incredibly rich data, significantly more information than is currently available, and also importantly, allows us to digitally mine this information for new quantitative biomarkers that can be really useful for both research and for individual clinical applications. A kind of summary is that we feel that we can take and importantly. Sorry, I will go back. I’m. And importantly, this this importantly this technology is doing that using existing infrastructure that’s already in every major hospital in the world right now. We use existing X-ray equipment. Existing CT equipment. Take the images from that and provide our analysis, our value add to take those still images and turn them into rich moving functional images. We would actually like to argue that this is the latest evolution of manufacturing. We are taking something that is of low value. We’re performing a process on it and we’re creating something that’s of much richer and high value. And we think that that’s really a sustainable type of manufacturing that Australia can compete internationally on. And so we have all of the advantages without the disadvantages of these these existing technologies. And you see the opportunities are really quite significant. Right. So I’m. In the United States alone, there’s $13.7 billion spent on these diagnostic tests every year right now. Really significant opportunities for Australian innovation to try to capture. So if I take a sort of small sidestep from the technology and just talk a little bit about myself and a little bit about my background, and you can see here a picture of a rather nice looking car sitting in a wind tunnel where it’s being used to measure, you know, to understand the air flow and so on. That’s happening over it. We want to see what’s the lift, what’s the drag, how much fuel with this car use and doing incredibly small things like changing the rearview mirrors can make a really big difference to that. That was my background as a as a mechanical engineering where I was doing my masters in at at Monash. I went from there to a career as a laboratory manager, and I found myself working in and around research, helping, helping other folks do their postgraduate studies. And I learned I learned a little bit, quite, quite a lot about doing that. And at one point I had the opportunity to interact, to cross-pollinate with what I was doing and to meet some folks in medicine and became really incredibly inspired about taking what I knew about measuring airflow and measuring resistance, drag and so on, and taking that and applying that to to inside the human body, inside the heart and inside the lungs. Now, you know, by that time I was married, I had kids. So I had to I had to take the the difficult step of deciding to do my postgraduate studies at night. So I’d work in the lab during the day, had access to the lab during the night and work through. And I spent about five years on about 2 hours sleep at night. And, you know, I learned a lot about prioritizing, prioritizing my my time. But at some point I hatched out of that really that that hard work, that really incredibly hard work for for that five year period really put a fire inside of me to really kind of take my academic career. And I really dreamed about becoming a, you know, a successful academic. And I guess that that passion and the strength of the technology that I developed allowed me to, you know, to have a fantastically some some really fantastic successes, a really great time as a as an academic and as a researcher that I will absolutely hold as, you know, real treasures for for for for the rest of my life. And just at the point where I thought, you know, after that sort of being, having to do all that night shift for all those years and then working my guts out to get to to full professor at the university, I thought I finally reached the peak and I realized actually that it really wasn’t what I wanted at all, that what I really wanted was to take the technology I developed and actually use it to to make a difference. So fortunately for me, some very understanding people around me in my life and I was able to, you know, to basically to to make that make that big decision, make that change and step step across sideways. So if I if I pivot now back to the technology, you know, as I showed that demonstration before, we are able to do some amazing things where we can measure airflow in people’s lungs, see where it’s going, see where it’s not going, create some really exciting biomarkers that are customized to particular research projects or particular diseases. But is it clinically useful? Does that actually help us to treat patients? You saw Amy story. He’s a he’s another example of and I think silicosis is is quite topical in Australia now. Occupational exposures are something that are very important to me and to our set at at 40. And you can see here a patient who was was exposed to to this, you know, this, this toxic hazard and had a really very significant impact on on their health. They had a CT scan which is this you know that black and white image on the left. And then the 40 medical scans, which are the colored images to the right hand side of that and the simple. Output of that is that in all of those images, we can see that there’s something wrong in that in those person’s lungs. What’s interesting is that person had an experimental therapy that’s being tried out. There’s some really fantastic work being done in Australia, globally leading the world in in treating these treating these conditions. And then had another CT scan, did the rest of the tests. And I didn’t see any change in those. We were able to to redo the the X-ray scans and we can really clearly see what’s happened. We can see that while the lungs haven’t changed their structure, they haven’t changed how they look, they’ve changed how they work as a result of that therapy. And that’s really critically important. Another exciting example, Here’s a patient who has a form of COPD and was put on once again put on an experimental therapy. Takes a long time to see whether these drugs work. There’s a lot of side effects. They’re incredibly expensive. Where I would say really quickly for which patients these drugs are working in, which patients these drugs are not working. Once again, really clinically very useful. And then finally, we we’ve seen Amy story. We can see that in long COVID, the technology can be used to detect, ah, these symptoms of long COVID because of something that’s in the lungs or is it somewhere else because there are other places it can be and if it is in the lungs, should we start them on treatment? Should we keep them on that treatment? Can we take them off that treatment? So multiple really important decision making points for that in that in that flow, I mentioned occupational exposure. You know, I’m you know, one of the things that’s been you know, that’s a real horror of of the 20 plus years of war that have been happening, you know, in the Middle East are these these burn pits. So the Americans decided that they should burn their rubbish and that that means, amongst other things, storing laptops, army boots, trucks, tires and whatever else into a into a hole in the ground. It can be that size or it could be the size of a of the MSG pouring jet fuel on top of it and lighting it on fire. And unsurprisingly, that’s not good for you. So there’s three and a half million American troops have been exposed to those burn pits. Many Australian troops have been as well, with doctors harder to see for Australians. And this is a there are many, many of these folks who have really significant health problems. As a result. We’re excited to say that we conducted a clinical trial with the folks at Vanderbilt University and with the the Department of Veterans Affairs in the United States, and we’ve had some really great successes. And the reason that this study was was necessary is these folks are not proving easy to diagnose. X X-rays do not detect the disease. Pulmonary function test is not to take the disease. CT does not detect the presence of this disease. So what’s become the standard of care with these folks or what’s become the only way to reliably detect the presence of this disease is literally cutting into their body. So cutting in three places in between the ribs, cutting a wedge of their lung tissue, putting sending that sample off to pathology for a pathologist to say if there’s something wrong there, it’s not fun. We see the scars in CTS many years after these procedures are performed. Takes three days to recover costs $15,000 and is generally not not fun and not the kind of thing anyone wants to do. We’ve been able to show that our technology can, with very high sensitivity and specificity, also detect the presence of that disease. So three and a half minute test, no pain and suffering a few hundred dollars instead of $15,000. And so this is something that we can really do to help those three and a half million folks. But also at the same time, there’s really significant opportunity on board for the Australian innovation sector to benefit out of this. Right At three and a half million folks, $200 a scan, there’s $700 million US of of export revenue available that could come into Victoria as a result of this this technology. So as I said, the transition was, was a very difficult one to ah to, to conceive of. But once I finally got there, I didn’t realize that that was really just the beginning of the of the pain and suffering associated with associated with that transition. The you know, I really required me to go all in. It required me initially to, to up the mortgage on my house and then eventually sell the house and then eventually borrowed quite a bit of money. And so I often tell people that my 40 medical shares are 115% of my net worth. And it’s really because actually, mathematically that’s true. I’ve got a massive amount of debt that, you know, even ten years as CEO of the company has hasn’t allowed me to to recuperate. So it’s there is that. You know, and my end, as you know, the family who was sitting there bored with that. But actually in some ways, some of the pain that hurt the most was really when the university told me that I just couldn’t be I couldn’t work at a university and run a business at the same time. The hypocrisy of it stunned me at the time. And then I guess when I realized as well that there’s no way I was ever going to go back, I’d sat on panels for the IOC in the NHMRC, and I knew no matter what the guidelines said, that I wasn’t going to win a grant after being out for a couple of years. It just wasn’t going to happen. So it was a one night trip into that into that frying pan and. You know this. I know they’re kind of the usual cliches, but I have on three separate occasions, had to put payroll on my credit card. So it really is true. It’s not just it’s not just us. It’s not just the story. Although the the time that hurt the most was calling my father in law to get payroll put on his credit card. I can tell you that that that one was was was really the most the most difficult of of all. So I’m. 40 Medical has an exciting pipeline of of new, innovative, new innovative technologies. We have our software products which we’re able to to layer, as I said, on top of existing X-ray machines and CT scanners. Everything I’ve talked about so far today has us measuring airflow in the lungs as people breathe. We’re excited about soon being able to add blood flow to that as well, and that’s going to really significantly add to the value of what we’re doing. Also, the MRI funded us out to the tune of $28.9 million to build a dedicated scanner. That’s very exciting and I’m very appreciative for the MRF to doing that. But I would like to point out that after we won that grant, our share price went down. So that’s, that’s what the the, the stock market thinks of, of innovative grant funding. So, you know, here is here Is that Skinner? We’re really very proud of it. This this is a platform that really can permanently revolutionize lung health. I have a dream that someone can sit down on on one of our scans. So firstly, sitting is a big innovation as opposed to lying down. And that for the radiation dose of less than one chest x ray in less than 10 seconds, that you can measure all the airflow and the blood flow in your lungs. And I think that that will give unprecedented power to doctors to see instantly everything in a quantitative fashion that’s happening inside of their patients lungs. And they can ask questions cheaply, easily and give them better information so they can make those better decisions. And here’s the part of the conversation where I have on one hand a huge amount of personal experience, but also zero qualifications. And so that that, you know, when I talk about policy, so be nice. So I think that I’ve cut this up into into three problems. We are we are forcing the rushing of these ideas. We are rushing ideas to be written down before they need to be. Then we are rushing them to be pushed out of the university into the world of business before they need to be. And then we are rushing them from being in unlisted private businesses to private businesses way, way, way, way earlier than they need to be. And that is hurting us every single step of the way. And I think one of the core components of it is just the lack of size and scope of venture capital in Australia compared to other places. On top of that, I could talk about policies that really discourage people from investing in things outside of, for example, real estate in Australia and so on. But, you know, I don’t want to turn this into a discussion about negative gearing tonight, but the but in all seriousness. When I was starting the company up, I had multiple people tell me that they could buy another house, another flat, or they could invest in my company. And they and they were really very confident which one was the right one to do. One of them was protected with great tax benefits and the other one wasn’t. So, you know, also we have some real cultural issues and they connected to the money issues as well. You know, one of them is in one of my very first meetings. You know, I admit that I had no idea what I was doing, but one of my first investor meetings are sitting down with an experienced head of investors. And at some point I said. You haven’t really properly introduced this guy over here on this conversation. Who’s who is this guy? And the investor said, Oh, that’s the person that if we invest in, you will replace you as CEO of the company. And I was like, Oh, you could have told me that at the start of the meeting. You know, I think there’s really just that. Whereas what I want to say, especially to those of you who who are coming from the inventors side of the equation, if I can call it that, if you are able to manage your ideas, to manage the people, to manage the money, to put it together, to perhaps write a grant application, to deal with a department head to do all of these things. If you can do those things, then they are all of the things that you need to do to be the CEO of a company. Let me tell you that. Please don’t ever, ever let someone tell you that you’re not able to do what it is you need to do. That’s a question for you. That’s a personal question for you, for you to decide. And, you know, I use the same trope all the time in terms of my pushback on that, to say, well, namely the ten most successful companies in all of history and tell me if the inventor and founder wasn’t the person who took that to that success. Oh, and I’m. If there’s some way I know it’s on a lot of other people’s lists. Anyway, it was on the previous page. I know it’s on a lot of other people’s lists, but we’ve got to find a way that we can let people move backwards and forwards. We absolutely have to do that. We’ve known that. We’ve got to find a way to do that. I’ll admit I don’t know how to find a way to do that, but that’s why there’s such incredibly smart people in this room and people are putting such great work into policy. We have to do that. It’s not that’s that’s not negotiable. And here it comes to the money as well. Money is really, really important. Right? And the. Our economy is losing trillions of dollars. The budget, you know. The budget is effectively the way I see this. A good analogy to see this is to imagine that we have a debt in this camp in this country that is costing the economy $100 billion a year of interest payments. And if you’ve got a problem, if you’ve got a credit card bill that is costing you $100 billion a year. You don’t solve that with a new $15 billion fund. It doesn’t. That’s that’s not what does it? You need to put an equivalent amount of money that pays off that debt so that interest goes away. That is that is the only way to do it. And we are absolutely missing zeros in terms of these problems. And I want to coin this phrase that we are slashing. We are smashing a sledgehammer with a walnut here. We are taking a very, very big problem and applying a very, very small solution to it. I don’t think that’s ever worked and I really don’t think it has scope to work with this with these problems that we have in front of us. So thank you so much. It’s been a real pleasure talking to you about these things.
Robert Klupacs [00:27:30] Congratulations on a fantastic speech and talk and I live part of that with you. And I’ve still got the scars and the journey we’ve had. A couple of quick questions for you come in. The first one we had from an anonymous, some people know you here. They said you were one of Australia’s youngest ever full professors. Looking back and you’ve talked about it a little bit, but what drove you to become an entrepreneur? What was the thing that made the click for me? You just said I’m not don’t want to be a full professor. I want to be an entrepreneur.
Dr Andreas Fouras [00:28:03] I think for me, I saw my natural skill and talent was in terms of the the inventive side, right? And that to me seemed well-suited to being in the university. And it but I, I met with venture capitalists, I met with captains of industry. So folks at GE and Siemens and and these other let’s you know not Australian companies. Right. And talk to them about what their appetite was to take our Australian technology and inject it into the international product pipeline. And it was nil. And so it was really only when I saw that the technology I developed would give me a, you know, an exciting career as an academic but wouldn’t really ever end up in health care helping people. And so, you know, it was it was just simply for me personally, it was I really wanted to see it done. And I was the only volunteer.
Robert Klupacs [00:29:01] When I say is a question here from Nicholas, how how do you manage conflicting board direction with visionary innovative decisions and how this is impact the effectiveness of your team?
Dr Andreas Fouras [00:29:15] Yeah, I think. My my father always used to say to me that life is the art of the possible. Right? And so you have to deal with the situation you have in front of you right here, right now. Right. And I think that’s one of the things that I like to say to doctors. You know, they should use the technology they’ve gotten from today to treat the patient they’ve got today. Right. And I think the same thing applies to me. It’s just that simple as well. You know, the. Have the good fortune of having eight and a half thousand investors who are supporting the company, you know, through the stock exchange with all of its imperfections. And, you know, Warren Buffett says that lots of people make the mistake that they think because they can buy and sell the shares that they should. You know, and that’s and that’s why I think that all of these great ideas shouldn’t be thrown onto the stock market. But but it you know, it creates it creates a set of challenges. We have we have that investment. We have the opportunity to get this done. And so, you know, we have to play within the rules of doing that. Now, You know, the truth is it’s a tremendous burden, and only right now is for getting to the point where it can weather those storms and get through it. But really, truthfully speaking, in the last few years, we haven’t been there and we’re fortunate to have survived all of those conflicting tensions. What we needed was some incubation. You know, I think, if you don’t mind me kind of going hard on this question, the you know, I’ve got I’ve got five kids and, you know, I’m trying to do the best I can to give them advice. And one of the things I try to say to them is to invest in yourself. But don’t don’t be in a rush, invest in yourself, build up what you can do, get an understanding of what it is you want to do, and then you can get out there and face life and try to make a show of it. And we do the exact opposite to our ideas in this country. We take them and say, Right, you’ve got 6 minutes to be profitable. Don’t worry about investing in yourself. Don’t worry about building up. So we just like be profitable tomorrow. And I think that’s the equivalent of taking our kids out of year nine and putting them in the salt mine to work, because making money this quarter is the only thing that matters. And we all know that, you know, you take someone, put them in the salt mine from the age of 13, they’re unlikely to make the same career earnings as a doctor at the end of it. Right. Sometimes that investment actually has a return. So, you know, I think that’s yeah.
Robert Klupacs [00:31:32] There’s a whole slew of questions. And I’m going to pick one of the ten here. Actually, this is the last one. They were going to sit in the panel and ask you a few more. This is from the re you had to go to the US. But what brought you back?
Dr Andreas Fouras [00:31:45] Yeah. So look, I’ll, I’ll clarify that. But so I think I’m absolutely truly in my heart. I am and have always will, you know, have always been and always will be an Australian. And the way needed to impress those investors, principally that we were focusing on our key market and that required me to show the leadership of be there being there in that key market. However, what I can tell you, 4D medical today employs about 140 people and 18 of them in there in the United States at every single opportunity, every time we can hire, we hire in Australia. And so we are overwhelmingly an Australian company, Australian investors, Australian company. And when we when we when we when we win these hundred million dollar contracts, these billion dollar contracts, that money will be flowing into, you know, our office or our business, which is just located, you know, just walking distance from here right now.
Robert Klupacs [00:32:39] Fantastic. Thank you very much.

Dr Andreas Fouras, Founder and CEO of 4D Medical.
Listen to other episodes of Med Tech Talks here