Med Tech Talks
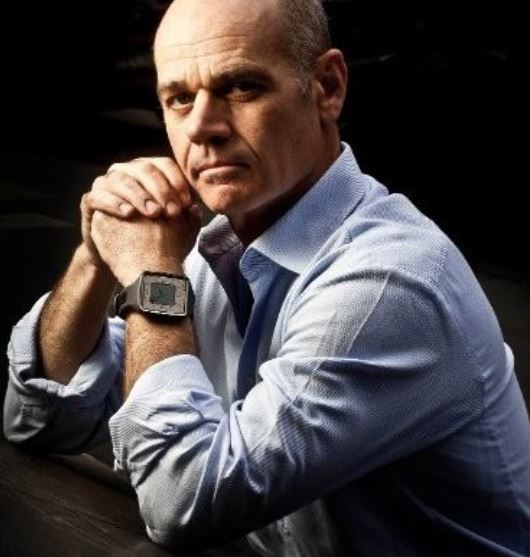
The Bionic Limb: an innovator’s journey with Max Ortiz Catalán

Professor Max Ortiz Catalán (Right), Head of the Neural Prosthetics Research Program at the Bionics Institute.
In additional to his role at the Bionics Institute, he is also the Founder of the Center for Bionics and Pain Research (CBPR) in Sweden – a multidisciplinary engineering and medical collaboration between Chalmers University of Technology, Sahlgrenska University Hospital, and Sahlgrenska Academy at the University of Gothenburg.
Professor Ortiz Catalán’s mission is to develop and clinically implement technologies to eliminate disability and pain due to sensorimotor impairment.
The Bionics Institute and CBPR are now working closely together to this mission.
In this episode you will hear about:
More information:
Learn more about Professor Max Ortiz Catalán
Professor Max Ortiz Catalán [00:02:03] Thank you for inviting me, Robert. A very kind introduction.
Robert Klupacs [00:01:58] Max Let’s go back to the very beginning. You have a very interesting CV, by the way, for all our listeners, and this will hopefully come out as we talk. You studied engineering and electronics at Tecnologia de Monterrey in Mexico and completed your PhD at Chalmers University of Technology in Sweden. What got you interested in bionic limbs and phantom limb pain?
Max Ortiz Catalán [00:02:21] I had a break in between those two. So I graduated from electronics back in Mexico in Toluca, and then I worked for the industry for a couple of years and I was working with sophisticated machines and vision systems for consumer goods, which on the technological side was interesting. But on, on a more personal side, it wasn’t really satisfying what I wanted to do in life. I decided to quit that job and go back to to school. Interestingly, I became fascinated by science late in my career, two years after I graduated from engineering. Not that early on when most people do, I wanted to build things. So that’s why that’s why I went to engineering. But then when I was just building things wasn’t enough. So I quit a good job. A few people thought I was a bit crazy and leaving the security of everything that was provided. But. But I just wasn’t happy. So I went back to be student. So I moved to Sweden and I stood at the master and complex adaptive systems, which are very interesting science, relatively new. And from there I for my master’s thesis, I wanted to do something in the medical field, and I was lucky enough that the field for integration was developed in Gothenburg Sweden where I was. So I get involved in that. So then I started working in that project and then. Then I ended up working on prosthetics.
Robert Klupacs [00:03:50] Fantastic. So I touched on what your research is a little bit in the intro, but for our listeners, can you explain exactly what you’re doing, what you’re developing, why what you’re doing is so important and what your you’ve done, which you think can make a major impact?
Max Ortiz Catalán [00:04:08] Sure. Prosthetic limbs. When people think about processes, they mostly think about the visible parts, the hard work, you know, the hands, sort of the legs that you can observe. But these are prosthetic systems. One part is the motors and the gears and the batteries. And then you have the human machine interface, the integration. How are those prosthesis connected to the body and how the person is controlling them? And it turns out that one of the major sources of problems for people with amputation is the connection between the prosthesis and the body. This is normally done with a socket. And what the socket does, it puts a lot of pressure on the receiver limb, on the on the soft tissues. And this you can think about an equivalent of this will be having very tight shoes that you have to wear to work the rest of your life. And that’s kind of the situation patients have with prosthesis. They have to have this very uncomfortable attachment that is put a lot of pressure in their soft tissues. They have to move around with it. When you move around, there’s friction between the skin and the device. If you see the limb is short, is not enough surface to grab. So then you have to block the adjacent joint that is healthy. But if you want to have a prosthesis attached, you need to sacrifice it. And then if it gets cold, it’s it’s a bit annoying, but if it gets warm, then you start sweating. And that can be very uncomfortable. If you gain weight, it doesn’t fit anymore. If you lose weight, it doesn’t fit anymore. So the fit in between that socket and your receive, the limb has to be very well done so you can have a better function. So that’s that’s something that is not very sexy to talk about, but that that is, in fact, one of the major problems. And what happened in Gothenburg in Sweden in the fifties by accident is one of those serendipitous moments in which a professor was doing experiments with titanium, trying to observe blood circulation in bone and realised that the titanium device he was using got stuck in bone. And that normally doesn’t happen because when you put a foreign object into the body, there’s a reaction by the body and there’s normally a fibrous tissue encapsulation because the body’s trying to protect itself and that makes it mechanically unstable. So it’s kind of easy to remove. And also your body will try to push out any foreign material if it can. But with titanium and bone, that doesn’t happen. So Bone says grow directly on titanium and makes a very strong mechanical attachment. So this is became much research filed and when I came to Sweden, this technology was used for mechanical attachment, which solves a lot of the problems that I described regarding the connection. But it doesn’t solve the problem of control.
Robert Klupacs [00:06:53] For our listeners. You founded the Centre for Bionics in Pain Research in Sweden, which is a multidisciplinary engineering and medical collaborations between the centres that I spoke about in the introduction. Can you tell me? Tell our listeners why you actually thought you had to Found a particular centre and what the mission is and how many people are working on it and how you think that could integrate with what you’re doing here at the Bionics Institute.
Max Ortiz Catalán [00:07:18] Sure. So when I was in industry the first years of my career and until not a long time ago, I had a foot in still in industry. But at some point I realised that academia could provide me the freedom that I like to develop ideas. So then I started at the laboratory. First it was the bio mechatronics and neuro rehabilitation lab, etc. So I got a small room and I had my students there and then that grew a bit quickly. Then they don’t have a space anymore. So it then I got a bigger room and then I just realised that what we wanted to do is create technologies that are used by people. And I’ve seen a common mistake back by biomedical engineers is that we as engineers would like to solve problems. So you will hear a medical problem and you’ll come up with a solution by yourselves and then bring it to the hospital. But it turns out that there’s some obvious usability design that you didn’t see because you’re not there and then then your development is useless and I didn’t want to do that. We had a good collaboration with clinicians and so on, but were separated from them, the hospital and all the engineers and it it can work but is not ideal. So at some point I said, well, if you know, if this is our full time job, we might as well go where the problem is and get embedded in the culture and the operations of the stakeholders so we can better understand the problems and develop technologies that are more useful. So then I approach the head of the departments. I was working with the director of the hospital, the Dean of the sequencing Academy in the university Gothenburg and I said, you know, why don’t we do this? Everybody like the idea. But it is it’s difficult to execute. However, I was fortunate enough to have a good relationship with the Promobilia Foundation, The Family Foundation. It’s a a foundation in Sweden that is dedicated to help to support the development of assistive devices to reduce disabilities, which is what I’ve been working for all my career. So we have known each other for many years and we discuss this project and they thought it will be meaningful and impactful. So they decided to finance it together with the Lundberg Foundation, which is another foundation in Sweden to provide the equipment. So then I raise what will that be in in the millions. So it was about 100 million Swedish crowns to for a five year period to run this this project. And then once I’ve raised that much money, was much easier for people to sign on the agreement. So once you have the funding, you knock on the doors and like, we want to do this, we have the money. And they’re like, Oh, sure, even though it’s still like that six months for for the agreement to be signed because, you know, these are big institution and so it requires quite a bit of perseverance there. But at the end we, we manage, so we move from the engineering facilities into the hospital so we could love space in the hospital. And then I start hiring not only engineers but also clinicians, because that was the whole point. One, to have a multidisciplinary team because we were working with them, but not necessarily financing all the activities. And once you once you have this the same I’m not sure it’s boss because that’s just not officially the right thing. But when you are funded for the same purpose is much easier to move forward because otherwise everybody has their own agendas and their own priorities and so on. And to develop complex medical devices is not an easy task and I think we see that all the time. And that’s why the development of medical device is slow. That’s why it’s you know, it’s already hard technically. But without having a close collaboration with clinicians. It’s just that it’s just not going to work.
Robert Klupacs [00:11:12] So you set that up. You had 100 million Swedish crowns, which I think is about $15 million Australian, a huge amount of money by our standards. It’s gone. The centre’s grown, I think. How many people now split? 30 people.
Max Ortiz Catalán [00:11:25] About it. It goes up and down depending on the students. So we we have to have students from abroad coming from from some periods we have visited. It is students and it goes up and down. Yeah.
Robert Klupacs [00:11:36] That’s going well. And then we reached out to you here at the Institute about 18 months ago and and said, look, this is what we’re doing. We really like what you’re doing. Can we form some type of link? And you’ve made the call to come and join us. What was the just for our listeners, what was it that you saw about the Bionics Institute that can help build on what you’ve already done at the centre? Because for our listeners, the Centre is still up and running, Max is still the Head of it, but he’s spending three quarter of his time here at the Institute. So perhaps you can tell our listeners what your vision is for that. Max.
Max Ortiz Catalán [00:12:10] Sure. That’s that’s an easy question. Firstly, it was a, you can say, almost love at first sight. I think the the values of the Bionics Institute and the passion, the purpose and my passion for translational research they just match was a very clear match from the beginning. I’m a pragmatic person. I became a professor not because I wanted to be a professor. Initially, that was not my childhood dream, but it but it was the means to achieve the impact that I wanted to. And then when I met, you know, you on the team and describe what the aim of the University Institute is, but not only with words, but what you guys have achieved with spinning off companies that are doing excellent work and hopefully they all will be successful. But even if they’re not all successful, if one or two of them are successful, that really makes a huge difference, you know, And that is that is something where we, you know, we done a lot of interesting things, but it’s still the translation I get. I’ve got a lot of first in human test and developments. So, I like to take ideas and bring them into a proof of concept where we can say, well, you know, this works, but that’s no longer enough for me. It’s just showing that it works. It’s no longer enough for me. I want to see it everywhere. And maybe not. You know, I want to it. It’s useful because that’s the point. And we have some technology that now we’re adopting for different things. So some of the work that I’ve done on pain that we’re using for stroke, rehab and nerve injuries and so on, but I’m always telling my my staff, this is not the silver bullet. You know, it should be used only where it’s useful. One, we mostly work on highly impaired subjects. Once there is some ability that there’s other technologies that are more useful than the ones that we work in with, for instance. So I try to keep in mind that the objective is to do something that is useful and that drive for for bringing things out that make things that are that are worthwhile and have a real world impact is what what attracted me. So I’m very happy to be here. And now that I’m, you know, have the opportunity to spend more time, it’s I’m even more convinced that it was the right choice.
Robert Klupacs [00:14:29] You made tremendous waves in the global research community in July of this year when you and your recent research team published the first documented case of an individual with an amputation above the elbow who was able to control a bionic hand as if it was their own. And I’d ask our listeners to look up Max on YouTube and see some of those videos. Just how big of a milestone was that for you and your team? And and what does this breakthrough mean for the future of people who will need your type of prosthetics?
Max Ortiz Catalán [00:14:58] Sure. So I will just give a brief history of how we got here and my masters degree thesis and then my PHD the was designing this implant that will allow a patient to control a prosthesis and I’m filled with it and the first patient that we that we publish a case study we shall we show that you know it was a stable it was for many years a patient just in daily life is actually more than ten years. Our first patient is using that system in daily life. So it’s an implant that’s on the bones, the skeletal attachment, the implanted electrodes. So when he thinks about doing a movement with his phantom or missing missing limb, the prosthesis response to that, and because the space, the physical space that he perceives his phantom to be is now occupied by the prosthesis he perceives as being its own hand. So that part, we had it working for over ten years now. Then the next step there was to to show that the sensory feedback was reliable over time. So we connect these electrodes in the nerves. So when we stimulate the nerves, the patients can feel sensations coming from the missing him. And it’s very interesting because you have biological, mechanical receptors of the kind of receptors and you say at your fingertips and those are connected to your brain via a nerve wire. And if you connect to that wire along the along the arm, know at any point it doesn’t matter what you stimulated. The brain will create the experience of the sensation coming from the fingertip. So this is very useful because now what we do is we connect to those nerves and we stimulate them and the patient feel sensations coming from the missing hand where now the prosthesis is. So they effectively feel the sensations arising from the prosthesis and this are very rough sensations, but are, you know, if you think about the development of a cochlear implant, the first cochlear implant had one channel and that didn’t sound like, like what, you know, what we consider sound to be, but it was much better than being deaf. So this is where we are with prosthesis. The sensations are very rough, not really natural, not not unpleasant, but functional or useful. So we show that in in a paper published in the New England Journal of Medicine in 2020, this patients had it for three years and then we started doing surgical reconstruction because we want to have the patients been able to control more degrees of freedom. So we combine artificial intelligence algorithms to the coding tension of movement together with rearranging the residual limb. So we move nerves and muscles and we bring muscles from other parts of the body to create a portal or access to more information and in the latest work that we published a couple of months ago. We did a surgery in which you take the nerves that used to go to the missing hand and and those come in in bundles and what you can do is to split those bundles, and then we transfer some of those bundles of nerves to muscles in the receiver that you think have a function. So if you, if you lose your hand, the both the elbow, biceps and triceps have not become a biomechanical function because there is no elbow to do to it. So we would transfer those nerves there. So when the patient thinks about moving the hand, those muscles contract. But we also more free from muscles grafts or small pieces of muscles from the leg to innervate those bundles. So when the patient thinks about doing movements with the hand, all those transfer muscles and native muscle contracts, we look at the pattern of activity of those muscles with artificial intelligence or machine learning algorithms, and then we know what the patient is trying to do. So we tell the prosthesis what to do and this allows for the first time to have a patient with an above elbow amputation to control every finger of a hand. In the same way they will control their prosthetic hand. So this is and this was a paper that we published now and we demonstrated in the lab. Now the next step is getting it to work in real world. So we were working on that. And again, now we have shown this is feasible in one person, but the challenge is to make it reliable and safe to be done in thousands or millions of people who have lost their limbs.
Robert Klupacs [00:19:11] Just to give me a flavour of that. So you’ve done it in one, but longer term. So you need to surgical techniques, you need to be healthy. So how long would it take for a person to undergo the surgery, recover, start using the limb and then start getting benefit from it in your own currently and then in the future. What do you think it would be?
Max Ortiz Catalán [00:19:32] It really depends on the person. If it’s a healthy young person, it goes much faster. You know, the bone quality is higher and so on. The nerve regeneration is faster. Typically with the current technology, if you get a nice integrated implant in the arms, you’re going to start using them in about three months because bonus, bonus living tissue. So if you if you lost a limb, that bone is not loaded, so becomes weak. And once you put the implant in, you start loading that you have to go slowly because you need to rebuild the strength that in that bone. So that’s a time that requires rehabilitation and then if you do nerve transfers. You need to wait for those nerves to grow into the new host targets or muscles or skin, depending on what we’re doing. So probably, you know, at least three months then. Then you started using it. And if you’re using muscles that are already there, it’s right away and if you already had a sense of the integration is right away. But the more complex the surgical procedure, then it takes a little bit longer. For, for instance, this patient, he had to remember how to control the missing fingers. Because he had the amputation for many years. Obviously, if you there’s something called learned paralysis. If you cannot move or you don’t have the limb, you stopped trying to do those movements, so you kind of forget how to do them.
Robert Klupacs [00:20:58] Interestingly, also integration, that centeredness really started to come into the realm of prosthetics. Over the last ten or 15 years. There’s been a bit of controversy with with the approach because a lot of people, the wound doesn’t heal when you put the titanium in planning to the bone. What’s your view about that and how do you think we can address that issue?
Max Ortiz Catalán [00:21:17] Yeah, so that’s been probably the main hindrance of the technology because you have this percutaneous crossing and there are different approaches to handle it. First system was the Swedish system and it was developed using the knowledge gathered from dental implants. So a lot of the and the bone anchors hearing aids and the surgical, the way you treat the skin around the bone and cause hearing device, for instance, was adopted in a way for for for limbs. And so, you know, try to to learn out of the different applications. So there’s you can say one approach in Sweden on how that’s done because of the the knowledge that existed before. Once all the integration started to become more popular than other people around the world started to create in their own system, mostly orthopaedic surgeons. And the common denominator there is that they’re very familiar with hip implants. All the other systems are basically an inverted hip implant. So there’s a mechanical stop and then this this long stem. And then there are some variation of that where where the skin sees the implant directly. In this Swedish approach, the skin consists can still see some of the bone, and there’s a discussion of whether that’s better for the skin interface or not, how you treat the skin and how you arrange the soft tissues. So this is an open problem. Still the function that patients get is is considerable. So everything is a trade off, right? We have patients that, you know, for whatever reason may lose their implant sometime, this antiseptic loosening and and they all welcome, maybe not all, but the big majority want to have it again, because the functionality that is the the stability we’re walking or not having a socket and not thinking about how much you have to work is just much. It’s a price. It’s a benefit that is worth the risk. And and you can see the same things with can transplantation, right, hand transplant can be very functional. But the drawback there is that the immunosuppressants that you need to take and the reduction in life expectancy. So to answer your question is it is an open problem is not a it’s not a showstopper because you still get much more function in upper limbs, it’s much less problematic than in lower limbs, for instance. And we have some some good ideas on how to solve it. So that’s what we’re going to be working on.
Robert Klupacs [00:23:43] Yeah. So just again, for our listeners, we’ve been speaking to people since you’ve been here and some people say, well, that’s, you know, an innovation. That’s not many. It’s not a big issue. Why are you spending so much time on it? So just for our listeners, can you put in perspective the number of amputations around the world that are happening? And I know with diabetes, it’s a number in the lower limb, but your focus in the arms but potentially in lower limbs. But just for our listeners, can you put it in perspective because the numbers, I think, will surprise many of them.
Max Ortiz Catalán [00:24:10] There was a study published a couple of years ago and they report that over 50 million worldwide due to traumatic injuries. So if you add those the amputations because of cardiovascular diseases, cancer and war, it becomes much higher. But it has never been a game of numbers for me because for those who have an amputation, it’s a big deal, right? And everything is relative, right? So this is a problem that I thought was worth spending my career working on. There is, in my perspective, enough people that can benefit from this work for me to dedicate my life to it.
Robert Klupacs [00:24:51] That’s fantastic. The other thing I want to touch on for our listeners, so we’ve been talking about new implants, new prosthetics for amputees, which is amazing, but in parallel, which is often amazing. You’ve also seen those same patients coming to you. One of the major issues with amputations in amputees is phantom limb pain, and they live with that daily. And apparently, I don’t know, fortunately, what it’s like, but apparently it’s incredibly debilitating. The other stream of your research that you’re doing is trying to overcome that phantom limb pain in amputees. Can you tell us a bit about what you’re doing and what you’re seeing and what your vision is there?
Max Ortiz Catalán [00:25:29] Sure. Phantom limb pain is it’s a horror. It’s a horrible condition. And the way I came into research, some phantom limb pain is because when I was doing the prosthetic work, I had to work with many patients who were helping me to develop, to test my algorithms that were kind enough to sit there and, you know, cut the electrodes and help me to test the the things that I was doing. And then I met a lot of wonderful people and one of them in particular was an a senior gentleman. And he was using this old prosthesis with with a with an old attachment and was 74, I believe, three at the time. And I said, you know, I’m developing this implant and it’s really cool. You have it attach it to the skeleton and you’ll be able to control the prosthesis well in July to change your current prosthesis to do this new technology. And he said, look, I’m fine with a prosthesis. My problem is pain. Like I couldn’t care less about not having my arm. But if, you know, if you can help me to stop the pain, that’s that’s what I mean. And then this become a more common occurrence. So and you know this like, if you’re in pain, nothing else matters. And of course, if you help them with pain, then they want a prosthesis, which is fine, you know, but priorities. Right. So this was I observed this when I was still doing my patches on my free time. I started working on this project. So actually, I had my first publication on phantom limb pain, I think before I graduated from my thesis. It was it was a parallel, kind of like a side hustle or an interest really, that became its own research branch. Now, because I realise it’s a it’s a big problem and there’s a lot of stigma around it as well. So not in all countries recognise and culturally some patients are concerned about reporting their pain because they might be considered crazy because if you think about it, how is it that you have pain in a part of the body that is no longer there? But it not only happens in extremities, you know, this is reported on on after mastectomies, you know, where the breast is removed. If you lose your nose and ear in different parts of the body. And it’s more common that what people think the majority of people with amputations of a body part, particularly limbs, will experience painful sensations. So before when I was speaking about prosthesis, I said that patients perceived their phantom or missing limb. Most people will do that, will still feel the presence of that body part. And then we can discuss, you know, why this is because of the way the brain is wire But the unfortunate reality is that sometimes those sensations are painful. It’s it’s a complex phenomenon. And I enter it on the practical side. So I had this technology and I read about it. So I figured that if we, you know, put some things together, we could maybe, you know, help this particular patient, which had pain. Pain is hard to hard to measure because it’s a subjective experience. So normally in clinically, you measure pain by asking the person how bad is the pain between 0 to 10 zero, no pain thing, the worst possible thing. And this person live most of his day in about a three level of pain and then he will have episodes of higher pain. And that was his life. So he had no period without pain. But when sleeping on his leg very poorly because of that. So then I developed this this system in which we will use electrodes to decode the intention of movement, similar as I was doing in prosthetics, but then use augmented reality, which is basically put a computer screen on a webcam and then the person can see themselves. And then we have the virtual limb where the where the missing limbs and the person can control it in the same way as they will consider the biological one. And by doing this and mixing mixing it with serious gaming, this patient and his pain reduced into the to the point where in one session. It was a very interesting. I love this story and this is just one of the stories of why I’m doing what I’m doing. So we we were trying this the risk and, you know, have we had ethical approval? Of course, and everything related to that. But it’s an exploratory a study. And then in the in the middle of a session, I saw that the patients start crying. So there were some tears coming off. So and I stopped and I said, are you having a lot of pain? Because sometimes it’ll have like a lot of pain. And and he said, no, this is the first time in 40 years that I don that I don’t have pain. And then from then on, his start experiencing periods with less pain and without pain, she started he started sleeping better, which improved his, you know, overall mood to the point where at the end of the of the treatment, his pain was no longer a factor in his life to the point where his wife basically told us, I think my my husband can live another ten years because pain is no longer there, you know, part of of the equation. And this is something that I was exploring, you know, on the side of my other big project on prosthetics. But I felt like. It will be morally wrong not to continue doing it, given the benefit so forth of this patient. So then I start making excellent efforts to to continue there. And then we tested it in patients with intractable chronic pain. They had pain for an average of ten years. And then we found similar results, about 50% decrease in pain in only 12 sessions. So if you think that you’ve been in pain for more than ten years and you need 12 sessions to cut it in half, it’s quite remarkable. So that was a study that was, you know, very rigorous and published in The Lancet in 2016. And the reason why we could publish it was because this was not my main research. So I didn’t want to spend my time on things that were not going anywhere. So I wanted to made it as extreme, as rigorous as possible. So if we had good facilities, it’s something real. It’s just not that this is not a fluke. The older I get, I suppose I’m even more careful on what I spend my time on. So I want to spend my time on things that matter. And this turned out to be something that had a real impact. So then I built a team and now it’s probably 50% of the work I do is focus on pain. But then we learned that technology. I started using it in patients with spinal cord injuries and what I saw that there were also functional improvements and I would use it in a stroke where we have very exciting results and that has grown to a few activities. And so now it’s a range of things. When establishing the Centre for Bionics and Pain Research, my aim and the mission of the centre is to eliminate disability costs by sensorimotor impairments. That’s and that’s kind of what we aim in. And when I, you know, came in contact with the Bionics Institute and you I saw that is, you know, it’s perfectly aligned. So, so now what we’re trying to do something is very exciting is leverage that know how from Sweden and Australia and the infrastructure and the infrastructure of the been extensive that is amazing. So it’s one of the main things that attracted me of course, leverage both the knowhow and the people in both places to make even bigger contributions.
Robert Klupacs [00:32:42] So do you think in ten years time using virtual reality, good electrode detection, that we can actually offer someone with pain, lower back pain, people with chronic pain for various conditions? Do we think we could really replace drug therapy potentially with some augmented reality systems?
Max Ortiz Catalán [00:32:59] Yeah. So that is one of the motivations In this first trial I run that was published in 2016, half of the patients reduce the medication by 50%. And I remember this particular patient that I met in in another city in Sweden, because that was a multicenter clinical trial and he had always a batch of morphine and then he had additional intake. So I remember meeting him. And and when you are in such high levels of opioid or, you know, you know, painkillers, you’re not yourself. You know, it takes it takes a little bit out of your it blunts you a little bit. And I remember meeting him after the trial when he was off the medication. It was entirely different person, you know, the character. It was a person who was alive. He was making jokes. It was like a different person. And I think, you know, for many patients with pain, what we have heard is that one of their objectives is stop having the medications because the side effects are are awful for you. They live, but they also make you dependent. So there’s a huge crisis on the opioid crisis you probably hear about in the U.S., for instance, where they use more than in Europe, certainly. So that’s a benefit. You know, sleep in better is a benefit because then your whole, you know, day goes better. And this side effects so far we haven’t seen any. So so this technology worst case scenario this can work but is not going to make you worse than what you were you know, at least from what what we seen.
Robert Klupacs [00:34:32] We’re running out of time with just two questions I want to touch on. One was for our listeners recently, Max was invited to the Ukraine and to actually meet people in a hospital, major rehabilitation hospital have heard about his work. Can you tell us what it was like to go into the Ukraine? Because most people haven’t been there hearing what’s going on and what you saw and why that was so interested in what you were doing?
Max Ortiz Catalán [00:34:56] Right. Yeah. So, you know, I’ve been saying that the reason why I’m getting all of this is is to make a contribution. And it was very clear that that there was this a big need for, for rehabilitation and post amputation pain in Ukraine. They expect to have more than 10,000 people with amputations by you know, by the end of the war, which hopefully sooner rather than later. So I visited a couple of months ago, visit a few hospitals in Ukriane. They over there, I saw more people with amputations than in my whole career. So the need was very clear. And I was very inspired by the level of commitment of the physicians they the surgeons and the rehabilitation therapies. They haven’t taken a day off since all this started. And they they do amazing job with with the resources they have available. Some of the technologies I develop are suitable for for some of the places. So I’m normally working on rehabilitation clinics where patients are stable and mostly working on the rehab. It was quite clear there’s a need for early rehabilitation. You know, once they just had their surgery because often they will spend weeks and months in in in a bed. You know, recovering from the injuries and war injuries are the worst poly traumas, very complex skin muscles, bone. Everything is is involved. There’s burn tissues it’s there are complicated which makes their the recovery more extensive which also means that often they can move and then the atrophy of those muscles even as you put everything together. So there’s this clearly a need to start narrowly rehabilitation and also to prevent pain. So what we are doing now, we had the proposal for this last project that hopefully will get funded soon in which we are we’re already adopting some of the technologies that we used to to do early interventions and also we trying to set up an instructional centre where surgeons in Ukraine can use some of the techniques that we use for rearranging their and reposition in tissue to to help to treat their patients, which is it is it is a complex situation because you need to be cost effective, time effective, efficient. You have limited resources, you have a lot of patients that need help and of course you want to do the best and that’s what we, you know, we’re trying to do. Again, we want to be helpful is is not a matter of, you know, have this technology. You should use it because we think is great. And one of the reasons why why I was personally there is because I wanted to analyse the logistics how what what is the patient path to care on how they go through the system. And I understood the different hospital types and how the patients are move through them, what are the resources at different hospitals and how we can make a more effective intervention at each location? So we’ll continue working there. I’ll be spend some time there and that’s more of that to come.
Robert Klupacs [00:38:08] Last question for you. If you were to give advice to any aspiring students or researchers about how they can maximise your their career. I mean, you you have come from an interesting path. What what insights would you give them?
Max Ortiz Catalán [00:38:21] Yeah, I often get the question from a students. I want to get involved in presentations and you know, how the how do I do the job that you are doing? And there is no one path, like many of my colleagues. We come from different backgrounds. My background is in electronics and algorithms, if you wish, but the world is sort of mechanical and some of the people are, by my usual advice, is identify what you’re good at and what you’re passionate about and become good at something. One discipline, you know, electronics or mechanics, computer science, medicine, whatever is excel at that one and they will open your doors. And once those doors are open, then you can decide how you want to move, because otherwise you rely on luck to get the positions you want. But if you if you are very good at something. Whatever it is that you want, then that’s personal. So you have to find that out. And there’s some good books. I mean, that beautiful thing about the time we live on is that people have done research about everything, you know, happiness and how you make a career. There’s some interesting there’s some very good books. We have a study how to do design, but not only design of things, but design of life. So there’s research on that even. So I think at this point we have no excuses for not, you know, educating ourselves to do our best professionally, but also life life wise and testing.
Robert Klupacs [00:39:40] Max, we’ve reached the end of our podcast today and I thank you for giving us your time and for sharing your research and your passion. And we really look forward to sharing exciting updates of your research in the near future and the next 12 months, 24 months, three years of your time. The institute’s going to be amazing. To our listeners, I hope you enjoy listening and I look forward to introducing you to other guests in future podcasts. There are links to everything we’ve talked about in the show notes and we look forward to welcoming you next time.
Listen to other episodes of Med Tech Talks here